The Complete Guide to Vitamin B6 Toxicity Symptoms—Even Without Supplements
Here’s the full spectrum of B6 toxicity symptoms—from neuropathy to mood and autonomic issues—even with low-dose intake and no supplements.
Why This Guide Matters
B6 Toxicity Symptoms are incredibly diverse and often quite insidious.
Most people assume vitamin B6 toxicity is only a problem for those taking megadoses of supplements. But that’s not always true. In reality, symptoms of B6 overload—such as tingling, nerve pain, insomnia, or mood instability—can appear in people with entirely normal intake, or even in those who have not supplemented any vitamin B6 for years.
This is the full spectrum of vitamin B6 toxicity symptoms, including cases where plasma PLP is elevated without any obvious cause.
While conventional medicine still treats B6 toxicity as rare, clinical and pharmacovigilance data suggest otherwise.
Vitamin B6 toxicity is extremely common, and many people’s mystery symptoms are due to insidious B6 toxicity, without their having any idea.
In the meantime, consider supporting my work by downloading the high B6 lab interpretation cheat sheet!
A growing number of people are developing sensory neuropathy, psychiatric symptoms, or unexplained autonomic issues—sometimes after taking only low to moderate doses of vitamin B6, and sometimes with zero identifiable source.
Unfortunately, many of these symptoms are misdiagnosed or dismissed.
This is the most complete symptom breakdown I’ve seen or used in practice, based on:
Published clinical reports
Biochemical mechanisms of B6 metabolism
Observed patterns in real-world patient presentations
If you're looking for a deeper understanding of how B6 overload occurs—even in people with “normal” intake—you absolutely must check out my Master Article on B6 toxicity. This article is part of a series I’m writing, based on the utter dearth of information on this veritable epidemic out there, and you’ll definitely want to read the original article in this series after this one:
AND ALSO NOTE that I’m in the process of building something far bigger than this article:
I’m working on a full B6 toxicity support platform that provides guidance on B6 toxicity that I haven’t found anywhere else. This will include deep dive videos as well as a private community where I’ll be present. The first 100 or so people will get locked-in beta pricing at around $50/month, though I’m still thinking through this. If you’re interested and you want me to update you when I launch this, share your email below:
This page focuses entirely on symptoms: what they are, why they occur, and how to recognize patterns that are often overlooked.
Common Signs & Symptoms of B6 Toxicity
Vitamin B6 toxicity doesn't present as a single disease—it shows up as a wide constellation of symptoms, many of which are easily mistaken for unrelated conditions.
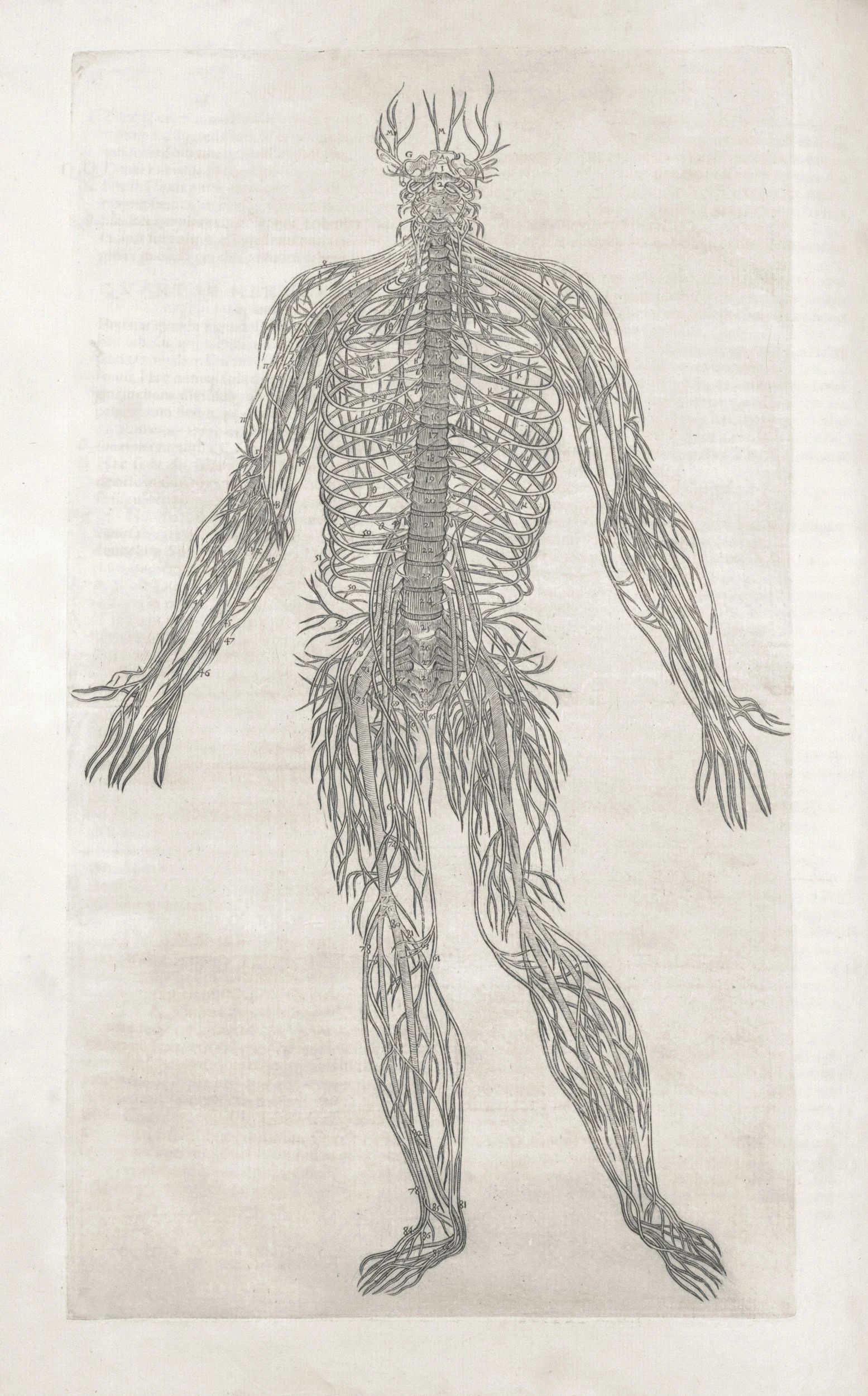
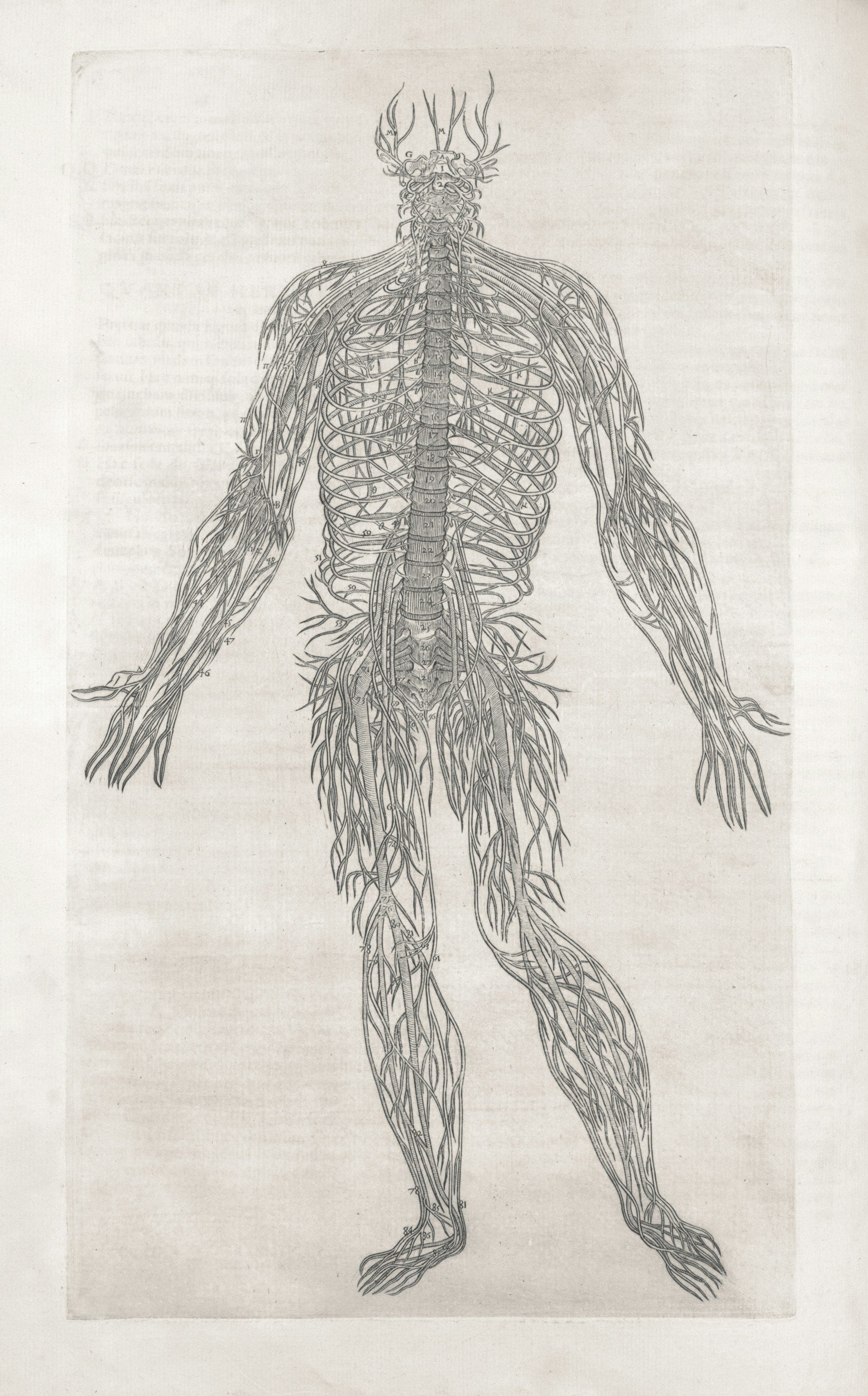
The most consistent and well-documented effects are neurological, affecting both large sensory nerves and smaller autonomic fibers.
What makes this especially important is that these symptoms of B6 toxicity can appear even in people who aren’t taking megadoses. Read about that here:
Large-Fiber Peripheral Neuropathy
Yes, B6 toxicity can affect both small as well as large fibers. Though symptoms usually begin with small fiber neuropathy, large fiber neuropathy can co-exist with small fiber neuropathy due to metabolic changes happening within nerve cells regardless of type and structure.
Large-diameter sensory nerves are responsible for position sense, vibration, and touch.
Common findings include:
Tingling, numbness, or burning in the hands and feet, often described as a "glove-and-stocking" distribution
Electric shock sensations or sudden jolts when tapping feet or fingers
Reduced vibration sense, especially at the toes or fingertips, detectable on clinical exam
Loss of grip strength, clumsiness when holding utensils, or difficulty with fine motor tasks
Balance issues or ataxia, sometimes without full awareness until walking is tested on uneven ground or in the dark
These symptoms are often progressive and can begin subtly. Many patients are misdiagnosed with diabetic neuropathy or told it’s just “age-related nerve irritation.”
That’s a major oversight.
In my experience, patients often sense something is wrong long before any diagnosis is made—particularly when tingling alternates with patches of numbness or when coordination issues start disrupting everyday tasks.
Small-Fiber Neuropathy and Autonomic Dysfunction
Small-fiber neuropathy affects thinly myelinated or unmyelinated fibers.
Typical sensory complaints include:
Burning, prickling, or buzzing sensations, especially at night or after heat exposure
Heightened sensitivity to clothing or bedsheets, especially in the lower legs or forearms
Paresthesias in the face, lips, tongue, or chest, often mistaken for anxiety or panic disorder
These are often accompanied by autonomic symptoms of B6 toxicity, such as:
Orthostatic intolerance—feeling faint when standing, or needing to sit down abruptly
Heart palpitations or racing heart rate when lying down
Abnormal sweating, including night sweats or complete lack of sweating during heat
Temperature dysregulation, such as sensitivity to hot showers, saunas, or cold air
Gastrointestinal dysmotility, including nausea, reflux, or alternating constipation and urgency
In some cases, the autonomic nervous system becomes so disrupted that symptoms mimic disorders like POTS (Postural Orthostatic Tachycardia Syndrome) or functional dyspepsia.
Patients are often told it’s all “just stress” or given SSRIs, which rarely help if the true root cause—in this, vitamin B6 toxicity—is not addressed.
Muscular & Movement Symptoms
While vitamin B6 toxicity is most often framed as a nerve problem, the downstream effects very often bleed into the muscular system as well. These B6 neuropathy signs—involving both nerve signaling and muscle responsiveness—can significantly impact quality of life, even when standard labs appear normal.
Muscle Symptoms of B6 Toxicity
When peripheral nerves misfire, muscles often respond with inappropriate or uncoordinated contractions. That’s why some of the earliest clues of a B6 problem show up in movement, muscle tone, and physical stamina.
Common complaints include:
Muscle twitching (fasciculations)—involuntary pulses or flutters, especially in the calves, eyelids, or hands
Leg cramps, especially at night or after minor exertion
Restless legs, a crawling or buzzing sensation that worsens at rest and improves with motion
Internal tremors, described as a shaky or vibrating feeling deep inside the body—often invisible to others but deeply uncomfortable
Unlike classic neuropathies where sensation is the only issue, these muscle-related B6 toxicity symptoms often arise from subtle disruptions in neuromuscular signaling. In other words, the nerve is misfiring, not “fried,” so to speak. Patients often describe a strange combination of hyperactive muscle activity alongside deep fatigue or heaviness in the limbs.
Fatigue and Motor Endurance Loss
In more advanced or prolonged cases of B6 overload, people may begin to notice:
Reduced stamina for walking or exercise, even if cardiovascular fitness is otherwise normal
Heaviness in the arms or legs, especially after extended use
Fine motor fatigue, such as hand shaking after short periods of writing, typing, or holding objects
These are not just signs of deconditioning. They’re often the result of impaired neuromuscular integration. When sensory feedback is blunted and motor firing becomes inefficient, even routine tasks can become exhausting.
Unfortunately, this pattern is often dismissed in younger patients as anxiety or “burnout,” and in older adults as just aging.
In my practice, these muscle and movement issues are among the most under-recognized indicators of a possible B6-related neuropathy—especially in patients who deny supplement use but still show elevated plasma PLP.
Mood, Cognitive & Sleep Disturbances
One of the more frustrating realities of vitamin B6 toxicity is how often it presents with psychiatric and neurologic symptoms that mimic unrelated conditions. People are frequently told they have anxiety, insomnia, or depression, but underlying reasons are never looked into.
Sleep Issues in B6 Toxicity
Sleep disruption is among the most common and least understood manifestations of B6 overload. And it doesn’t always look like classic insomnia.
Patients often describe:
Difficulty falling asleep, with a racing mind or a wired-but-tired feeling
Early awakenings, especially in the 3–4 a.m. range, with an alert surge or palpitations
Vivid or disturbing dreams, sometimes escalating into night terrors
Restless sleep—not deeply refreshing, even after enough hours in bed
This isn’t just poor sleep hygiene. In cases of elevated plasma PLP, the brain appears to remain hyperstimulated at night, likely due to dysregulated neurotransmitter clearance or GABA-glutamate imbalance.
Mood Symptoms of B6 Toxicity
B6 is essential for neurotransmitter metabolism, including serotonin, dopamine, and GABA. When B6 metabolism is deranged (read about that here), mood regulation often becomes unstable. In my clinical work, common patterns include:
Sudden waves of anxiety or agitation, especially out of proportion to external events
Unpredictable mood swings—calm one moment, irritable or teary the next
Episodes of panic, often without a clear trigger
Depersonalization or derealization—feeling detached from one’s surroundings or self
These symptoms often interfere with relationships, work, and emotional stability. And in people with no psychiatric history, the sudden onset is often striking and incredibly worrying.
Cognitive & Sensory Processing Changes
In addition to emotional dysregulation, many patients experience cognitive symptoms that are often dismissed or misattributed:
Brain fog, described as slowed thinking, blankness, or inability to focus
Sensory overload—difficulty tolerating lights, sounds, or busy environments
Tinnitus or internal buzzing, sometimes constant, sometimes intermittent
Reduced short-term memory or word-finding difficulties
These changes don’t just happen to older adults. Many of my younger patients—especially those with underlying metabolic sensitivity—experience these symptoms at the peak of their B6-related dysfunction. They often correlate with elevated plasma PLP levels (but NOT ALWAYS, very importantly) even supplementing B6.
Gastrointestinal & Systemic Symptoms
Although vitamin B6 toxicity is often framed as a neurological issue, it can just as easily affect the gastrointestinal tract and broader systemic function (though these effects are generally secondary to neurological effects). These symptoms are often overlooked or misattributed to unrelated GI disorders, yet they show up consistently in patients with confirmed B6 overload.
Gastrointestinal Distress from B6 Toxicity
Many patients report:
Nausea, often vague and persistent, without a clear food trigger
Upper abdominal discomfort or burning, especially post-meal
Intermittent bloating or fullness, even with small meals
Cramping, particularly in the lower abdomen
These symptoms are often dismissed as reflux, IBS, or anxiety-related gut “tension.” But GI symptoms often resolve only after elevated B6 levels normalize, suggesting a direct link between plasma PLP elevation and enteric nerve irritation.
Visceral and “Internal” Sensory Symptoms
Another under-recognized pattern involves vague, hard-to-localize sensations that patients struggle to describe but which often follow the same neuropathic distribution seen in peripheral nerve issues:
Internal tingling, sometimes described as a buzzing or fluttering feeling in the stomach or chest
Dull, nerve-like pressure in the abdomen, often worse at night or when lying down
Sensations of movement or agitation in the gut, with no corresponding GI findings
These symptoms are best understood as a form of visceral sensory neuropathy, where small-fiber nerves within internal organs become sensitized. In the context of B6 toxicity, this is likely due to disrupted sensory signaling caused by excess or poorly processed PLP.
Appetite and Weight Changes
Less commonly, patients may experience:
Loss of appetite without depression or GI obstruction
Unintentional weight loss
Food aversions, often tied to the onset of symptoms
While these signs are nonspecific, they appear more frequently in patients with higher B6 levels and overlapping neurologic symptoms.
Rare but Key Under‑Recognized Symptoms
Some of the most revealing signs of vitamin B6 toxicity are also the ones most frequently missed, precisely because they fall outside the conventional neurological picture.
These symptoms may be misdiagnosed as anxiety, aging, hormonal shifts, or simply ignored altogether. But in patients with elevated plasma PLP and a corresponding array of symptoms, these so-called “soft signs” can be the earliest or most persistent indicators of subclinical B6 overload.
Nighttime Cold or Burning Feet
Some patients report a very specific complaint: their feet feel icy cold or intensely hot, especially when lying down at night. This is not due to circulation loss or ambient temperature, but likely reflects small-fiber sensory nerve dysfunction, affecting temperature perception and regulation. It often resolves as B6 levels normalize.
Phantom Crawling or Itching Sensations
Another poorly understood feature is the sensation of crawling, prickling, or itching on the skin, typically without visible rash or irritation. These paresthesias can occur on the legs, arms, scalp, or torso. Some patients report feeling as though insects are moving on the skin or that their skin is being lightly “zapped.” These are classic signs of neuropathic sensory misfiring, and they’re pretty frequent with B6 overload.
Emotional Lability and Tearfulness
Beyond anxiety or depression, a subtle but notable pattern involves increased emotional sensitivity, particularly tearfulness without clear triggers, sudden weepiness, or rapid mood swings. This emotional lability may reflect deeper neurotransmitter disruption (serotonin, dopamine) in the context of B6 toxicity, and it’s often overlooked in the absence of overt psychiatric disease.
Impaired Proprioception
Some individuals with B6 toxicity lose the sense of where their limbs are in space, especially in the dark or with eyes closed. This can lead to:
Clumsiness in low light
Difficulty placing feet while walking
Needing visual cues to coordinate movement
This is known as proprioceptive loss, and while rare, it tends to occur in more advanced or long-standing cases of large-fiber neuropathy.
Bladder or Urinary Changes
Though not widely discussed, some patients also report:
Increased nighttime urination
Bladder urgency or mild incontinence
A subtle loss of sensation during voiding
These symptoms likely reflect autonomic nerve involvement, affecting the bladder’s sensory and motor regulation.
Symptom Onset & Progression
One of the most deceptive aspects of vitamin B6 toxicity is its slow, insidious progression. Unlike other nutrient toxicities that produce abrupt symptoms at very high doses, B6 overload very often (but not always) emerges extremely gradually, even in people taking seemingly modest amounts, sometimes as low as 2–5 mg per day from multivitamins or fortified foods.
Onset: Slow and Subtle
Again, in most reported cases, symptoms appear gradually over several weeks to months of daily B6 exposure. Early signs—such as tingling in the feet, mild insomnia, or mood shifts—are easy to dismiss or attribute to unrelated causes and often are only recognized in hindsight.
This is particularly true in individuals with:
Low nutrient status
Mild kidney or liver impairment
Underlying genetic vulnerabilities
Chronic use of multivitamins, protein powders, or energy drinks
In contrast, acute toxicity from high-dose supplements (e.g., 100-500 mg per day or more) generally yields more rapid onset of symptoms (within days to weeks, or less).
Coasting: Why Symptoms May Worsen After Stopping
A common and underappreciated feature of B6 toxicity is the phenomenon of “coasting,” where symptoms persist or even temporarily worsen after B6 intake is discontinued. This occurs for several reasons:
Plasma PLP has a long half-life, especially in tissues like nerve cells
Damaged peripheral nerves may continue to degenerate for a time after exposure ends
Nervous system repair takes time, and metabolic balance needs to be restored gradually
This delayed trajectory is typical.
Recovery
Recovery from B6-induced neuropathy can take several months, depending on severity and duration of exposure. In milder cases, patients may notice early improvements within 4-6 weeks of stopping all B6 sources. In more entrenched cases, full neurologic recovery may take 6–12 months or often years, especially if symptoms were present for a year or more before diagnosis.
That’s the case for simple B6 withdrawal.
However, a more targeted approach absolutely can yield much quicker recovery, often orders of magnitude quicker (more on that in other articles).
Why B6 Toxicity Often Gets Misdiagnosed
Symptom Overlap With Other Diagnoses
The neurologic and psychiatric manifestations of B6 overload closely resemble those of several far more commonly discussed conditions:
B12 deficiency – both cause distal neuropathy, gait instability, and mood disturbance
Diabetic neuropathy – tingling, burning pain, numbness in feet and hands
Fibromyalgia – sensory sensitivity, fatigue, nonspecific pain
Multiple sclerosis – ataxia, paresthesias, visual changes in advanced B6 cases
In such cases, clinicians often pursue more serious diagnoses—neurology referrals, MRI scans, autoimmune panels—before considering the possibility of a vitamin toxicity. This leads to diagnostic delay or misattribution.
Psychiatric Mislabeling
In many patients (especially women) B6 toxicity first presents with insomnia, restlessness, anxiety, or mood instability. When there is no overt neurologic deficit, these symptoms are often interpreted as psychological in origin.
Patients may be prescribed SSRIs, benzodiazepines, or sleep aids rather than having their supplement history and B6 intake reviewed.
Extremely importantly, in some cases, the B6 itself is part of a “mood support” stack, further confusing matter.
Lab Results Are Misread
Even when plasma B6 is tested (typically measured as PLP, or pyridoxal-5'-phosphate), results in the upper-normal or mildly elevated range (e.g., 50-100 or so nmol per L) are frequently dismissed.
Many clinicians are unaware that symptoms can occur even within the so-called normal range, especially if the patient has nutrient deficits or genetic impairments that affect intracellular B6 processing. Some patients may even have paradoxically normal serum B6 because of impaired tissue uptake or distribution.
(Learn the first steps toward interpreting your high B6 level with my cheat sheet):
B6 Toxicity Is a Major Knowledge Vacancy
Finally, most doctors simply don’t consider B6 toxicity in their differential diagnosis at all. It isn’t covered in depth (or sometimes at all) in medical school or residency—I’ve been through that training myself.
And because it's a water-soluble vitamin with a generally safe reputation, it’s usually considered totally innocuous.
I’ve seen many well-documented cases of B6-induced neuropathy occurring at doses between 2-50 mg/day, often from multiple hidden sources: a multivitamin, protein shake, energy bar, and “stress formula” all stacked together.
Why Symptoms Appear with No Supplements
One of the most overlooked realities of vitamin B6 toxicity is that symptoms often emerge even when a person isn’t “supplementing.” Many of my patients insist they aren’t taking B6, yet their plasma PLP levels are elevated, and their symptoms fit the classic profile of toxicity.
Read my article on that:
Clinical Pathway: What to Do Next
Attempting to treat this without full biochemical context is highly likely to cause more harm than good, or at the very least to be highly suboptimal in efficacy.
Here’s a structured clinical approach:
1. Cut *every* source of B6
Stop all multivitamins, B-complexes, protein powders, fortified foods, and drink mixes
Review all supplements and medications for hidden B6 content (including “natural” blends)
2. Order Core Laboratory Testing
Plasma PLP (pyridoxal-5′-phosphate)—the active form of B6
Comprehensive nutrient testing (easier said than done)
Liver and kidney function markers
These establish the central picture: is B6 truly elevated? Are processing cofactors impaired? Is elimination compromised?
3. Consider Advanced Evaluation (Clinician-Directed)
Assess clearance vs. conversion
Genetic testing for subtle variants in B6 metabolism (e.g., phosphorylation, dephosphorylation, transport)
Neurological and autonomic testing, if significant nervous system signs are present
Etc.
And, of course: don’t assume symptoms will resolve quickly just by stopping supplements.
Why This Is a Precision Medicine Issue
Vitamin B6 toxicity highlights a broader truth in clinical nutrition: there is no universal safe dose.
While the RDA (Recommended Dietary Allowance) is designed to meet the needs of most healthy individuals, it does not account for outliers—people with subtle genetic, metabolic, or elimination-based vulnerabilities. For these individuals, even so-called “normal” intakes (as low as 2 mg per day, or even less) can result in bona fide toxicity and symptoms.
Certain individuals cannot clear B6 efficiently, leading to sustained plasma elevation despite low intake
Cofactor deficiencies can block conversion or breakdown pathways
Variants in enzymes or transporters involved in B6 metabolism can impair intracellular utilization and excretion
Underlying mitochondrial or liver stress may further suppress processing capacity
In clinical terms, this means the threshold for toxicity must be personalized. What’s safe, or even essential, for one patient may be harmful to another.
That’s why I consider B6 toxicity a precision medicine problem: It demands metabolic profiling, highly precise nutrient analysis, and individualized dose thresholds, not population-based assumptions.
If you want to work with me personally: let’s talk.
Frequently Asked Questions
-
Yes, absolutely. In sensitive individuals with impaired clearance, even 1–2 mg from fortified foods, multivitamins, hydration powders, etc. can cause symptoms, especially with concurrent nutrient deficiencies, genetic deficits, etc. Read more here.
-
Subtle tingling in the feet, restless legs at night, or unrefreshing sleep are very often the earliest clues, especially if they come on gradually and without clear cause.
-
Mild cases may improve within 4–6 weeks after stopping all B6 sources. But full nerve recovery can take 6–12 months, or even years, especially if symptoms were present for a long time. Much, much faster recovery (orders of magnitude difference) can be obtained via a precision medicine approach, however.
-
There is no single test that confirms it to date. B6 levels in the plasma/serum can be completely normal even with B6 toxicity, and vice versa. It’s a highly multifactorial, syncretic analysis.
-
This “coasting” effect happens because nerves take time to heal, and PLP can remain elevated in tissues for weeks, months, or more. Symptoms often peak before they improve.
-
Yes. Fortified foods, protein powders, and energy drinks often contain hidden B6. If your metabolism or clearance pathways are impaired, even this background intake can cause toxicity. Read more here.
-
Look for tingling, buzzing, balance issues, vivid dreams, palpitations, or anxiety that doesn’t respond to standard treatment—especially if plasma B6 is elevated.
-
Yes, without a doubt. Though the particular genes causing such susceptibility are highly idiosyncratic.
-
Absolutely. This is a nuanced topic. Read more about that here.
Read more: